In the evolving landscape of personalized medicine, understanding one's genetic predisposition to osteoporosis has become a cornerstone of proactive health management. This silent disease, characterized by weakened bones and increased fracture risk, often goes undetected until a devastating break occurs. Emerging research reveals that our genes play a significant role in determining bone mineral density and overall skeletal resilience. While we cannot change our DNA, sophisticated genomic insights now empower individuals to craft targeted defense strategies against this brittle bone threat.
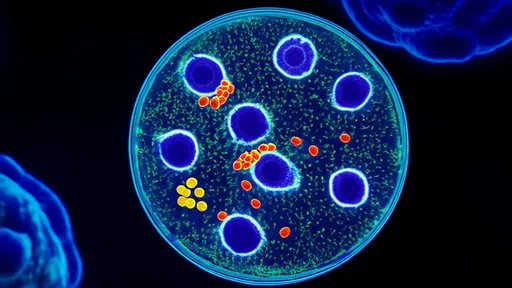
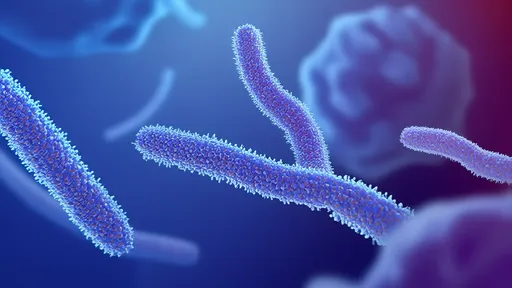
The Genetic Blueprint of Bone Health unfolds through complex interactions between multiple gene variants. Scientists have identified over 60 genetic markers associated with osteoporosis risk, with the most significant found in genes governing vitamin D metabolism, collagen production, and bone remodeling processes. The VDR gene variants influence how efficiently our bodies utilize vitamin D, while COL1A1 polymorphisms affect type I collagen quality - the protein scaffolding that gives bones their tensile strength. Perhaps most crucially, variations in the LRP5 gene can dramatically impact bone mineral density regulation.
Modern genetic testing services now screen for these critical variants through simple saliva samples, offering unprecedented windows into personal bone health vulnerabilities. However, possessing high-risk alleles doesn't equate to an inevitable osteoporosis diagnosis. Rather, these genetic insights serve as powerful motivators for implementing precisely tailored prevention protocols. Individuals carrying the VDR BsmI variant, for instance, may require significantly higher vitamin D supplementation to achieve optimal bone protection compared to those with standard genotypes. Nutritional Countermeasures Against Genetic Risk begin with calcium optimization, but the approach must extend far beyond basic supplementation. Those with COL1A1 risk alleles often benefit from increased silicon intake through foods like bananas and whole grains, which supports collagen formation. Magnesium becomes particularly crucial for individuals with CASR gene variants that impair calcium sensing. Emerging research highlights the importance of vitamin K2 for proper calcium deposition in those with OPG gene polymorphisms, directing the mineral toward bones rather than arteries. Strategic exercise programming forms another critical pillar of genetically-informed osteoporosis prevention. While weight-bearing activities universally benefit bone health, individuals with high-risk LRP5 variants may require more intensive resistance training to stimulate adequate bone formation. Surprisingly, research suggests those with certain FGF23 gene mutations respond exceptionally well to vibration plate therapy. Tailoring workout regimens to one's genetic profile transforms exercise from a generic recommendation into a precision medical intervention. Beyond nutrition and activity, environmental factor modulation plays an underappreciated role in mitigating genetic osteoporosis risk. Night shift workers carrying the CLOCK gene variant show accelerated bone loss due to circadian disruption, making sleep hygiene paramount. Individuals with GSTP1 polymorphisms exhibit heightened bone sensitivity to environmental toxins, necessitating rigorous air and water purification. Even simple measures like maintaining stable indoor temperatures can benefit those with TRPV5 calcium channel variants that impair thermal regulation of bone metabolism. The psychological dimension of genetic risk awareness warrants equal consideration. Learning one carries high-risk alleles can initially provoke anxiety, but reframing this knowledge as empowerment transforms the narrative. Support groups specifically for individuals with osteoporosis-related gene variants have emerged, fostering communities where members exchange personalized strategies and celebrate small victories in bone density improvement. This psychosocial support proves particularly valuable when navigating the complexities of genetic risk without succumbing to deterministic thinking. As research progresses, cutting-edge interventions continue emerging for those at highest genetic risk. Precision pharmaceuticals like sclerostin inhibitors show particular promise for individuals with WNT pathway mutations. Novel nutraceuticals such as strontium citrate demonstrate enhanced efficacy in those with specific calcium receptor gene variants. Even low-frequency electromagnetic field therapy has shown genotype-dependent effectiveness in clinical trials. The future of osteoporosis management lies not in universal protocols, but in these highly individualized approaches informed by each person's unique genetic architecture. Ultimately, genetic knowledge transforms osteoporosis from a fate to a manageable variable in one's health equation. While DNA provides the blueprint, lifestyle writes the story. Those armed with understanding of their genetic vulnerabilities gain the power to implement targeted, evidence-based strategies that often prove far more effective than generic advice. In the dynamic interplay between genes and environment, proactive individuals retain remarkable influence over their bone health destiny.
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025