Morning blood pressure surges have long been recognized as a critical factor in cardiovascular health. Unlike the relatively stable readings taken in clinical settings, the early hours after waking often reveal dramatic fluctuations that carry significant prognostic value. These transient spikes, sometimes called "morning surge," correlate strongly with adverse events like stroke and myocardial infarction. Understanding the mechanisms behind this phenomenon and learning to mitigate its effects could mean the difference between controlled hypertension and catastrophic organ damage.
The human body operates on a finely tuned circadian rhythm that influences nearly every physiological process. Blood pressure follows this pattern with a characteristic dip during sleep and a sharp upward trend upon awakening. This natural escalation becomes problematic when exaggerated, placing undue stress on the arterial walls. Research indicates that the morning surge involves complex interactions between the sympathetic nervous system, endothelial function, and hormonal cascades. Cortisol and catecholamines peak during these hours, while impaired baroreflex sensitivity fails to adequately compensate for the rapid changes.
Environmental triggers play an underappreciated role in amplifying morning blood pressure variability. The simple act of rising from bed creates orthostatic stress, while morning routines often include caffeine consumption, nicotine exposure, or strenuous activity. Cold bedroom temperatures during winter months may further exacerbate vasoconstriction. Many patients make the critical error of measuring their blood pressure after breakfast or coffee, completely missing the diagnostic window when surges typically occur between 4-10 AM.
Medication timing represents one of the most modifiable factors in controlling morning fluctuations. Conventional once-daily antihypertensive regimens frequently fail to provide adequate coverage during the early morning hours. Studies demonstrate that taking certain medications at bedtime rather than morning significantly improves morning blood pressure control without compromising nocturnal dipping. This approach appears particularly effective with ARBs, ACE inhibitors, and some calcium channel blockers, though individual response varies considerably.
Dietary modifications extend far beyond simple sodium restriction when addressing morning blood pressure dynamics. Potassium-rich foods consumed the previous evening appear to blunt morning surges, possibly by modulating sodium-potassium pump activity overnight. The gut microbiome's fermentation of resistant starches produces short-chain fatty acids that influence autonomic regulation. Emerging evidence suggests that tart cherry juice or hibiscus tea taken before bed may attenuate morning blood pressure through flavonoid-mediated mechanisms.
Sleep architecture profoundly influences next-morning blood pressure profiles. The transitional period between deep sleep (N3 stage) and REM sleep triggers microarousals that activate the sympathetic nervous system. Patients with untreated sleep apnea experience repeated oxygen desaturations that intensify morning surges. Even among healthy individuals, poor sleep efficiency or late-night alcohol consumption can disrupt normal blood pressure dipping patterns, leading to exaggerated morning increases.
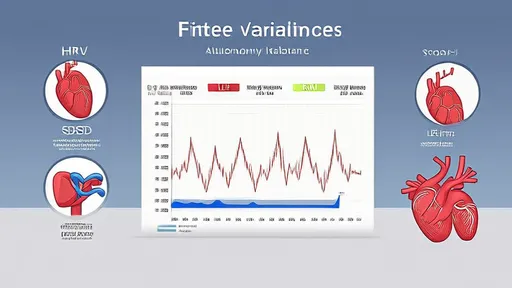
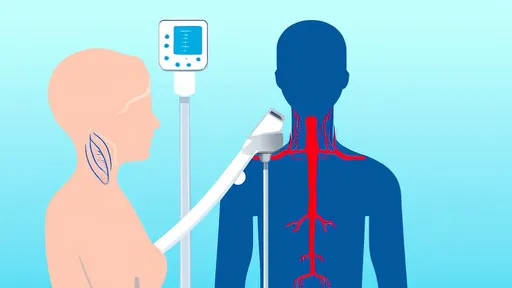
Technological advancements now allow for more precise monitoring of morning blood pressure patterns. Traditional 24-hour ambulatory monitoring often misses critical fluctuations, while newer wearable devices can capture beat-to-beat variability. Smartphone-connected home monitors with position sensors help distinguish true surges from measurement artifacts caused by improper cuff placement or arm position. These tools empower patients to identify personal triggers through longitudinal tracking.
The psychological dimension of morning blood pressure management deserves equal attention. The anticipatory stress of upcoming daily challenges can create a conditioned blood pressure response before patients even open their eyes. Mindfulness practices upon awakening may help short-circuit this physiological cascade. Simple techniques like controlled breathing for five minutes before getting out of bed have shown remarkable efficacy in clinical trials.
Exercise timing presents a double-edged sword for morning blood pressure control. While regular physical activity generally improves cardiovascular health, intense morning workouts may trigger dangerous spikes in susceptible individuals. Conversely, evening resistance training appears to confer protective effects that persist through the next morning. The warm-up duration and hydration status before exercise further modify these responses.
Individualized medicine approaches are revolutionizing morning blood pressure management. Genetic polymorphisms in clock genes, adrenergic receptors, and sodium channels help explain why some patients experience extreme surges while others maintain stable readings. Pharmacogenomic testing can guide medication selection, with certain beta-blockers proving more effective for patients with specific genetic profiles. This precision medicine paradigm moves beyond one-size-fits-all treatment algorithms.
Clinicians often overlook the importance of educating patients about proper morning measurement techniques. Readings should be taken within one hour of waking, before medication but after voiding, with the arm supported at heart level. Patients must avoid talking or crossing legs during measurements, as these common behaviors can artificially elevate readings. Establishing these protocols ensures accurate data for clinical decision-making.
The vascular endothelium functions as both victim and perpetrator in morning blood pressure dysregulation. Nocturnal repair processes become interrupted by premature activation of inflammatory pathways, leaving blood vessels vulnerable to morning hemodynamic stress. Biomarkers like asymmetric dimethylarginine (ADMA) may help identify patients whose endothelial dysfunction predisposes them to exaggerated morning surges.
Seasonal variations in morning blood pressure patterns necessitate adaptive management strategies. Colder months typically see higher morning surges due to peripheral vasoconstriction, requiring closer monitoring and possible medication adjustments. Indoor heating systems that create dry environments may contribute to nocturnal dehydration, further complicating morning hemodynamics. Patients living in regions with dramatic temperature swings may benefit from more frequent treatment regimen reviews.
Integrative approaches that combine chronotherapy, lifestyle modification, and advanced monitoring offer the most promising path toward taming morning blood pressure volatility. As research continues to unravel the intricate mechanisms behind morning surges, clinicians gain increasingly sophisticated tools to protect patients during these vulnerable hours. The ultimate goal extends beyond numerical blood pressure control to preserving vascular integrity throughout the circadian cycle.
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025