In the modern era of sedentary lifestyles and processed food consumption, insulin resistance has emerged as a silent epidemic affecting millions worldwide. While pharmaceutical interventions exist, a growing body of research highlights powerful non-pharmacological approaches to enhance insulin sensitivity. These natural strategies not only improve metabolic health but often address root causes rather than just symptoms.
The human body's relationship with insulin is complex yet remarkably responsive to lifestyle modifications. When we talk about improving insulin sensitivity without medication, we're essentially discussing how to make our cells more receptive to insulin's signals. This biological responsiveness forms the foundation for preventing and even reversing conditions like prediabetes and type 2 diabetes.
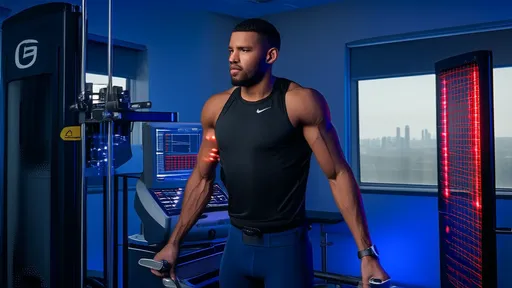
Physical activity stands as one of the most potent natural insulin sensitizers. Movement creates a demand for energy that prompts muscles to efficiently uptake glucose, independent of insulin. This effect isn't limited to intense workouts—consistent moderate exercise and even regular walking can significantly impact insulin sensitivity. The mechanism involves increased translocation of glucose transporters to cell membranes and improved mitochondrial function in muscle cells.
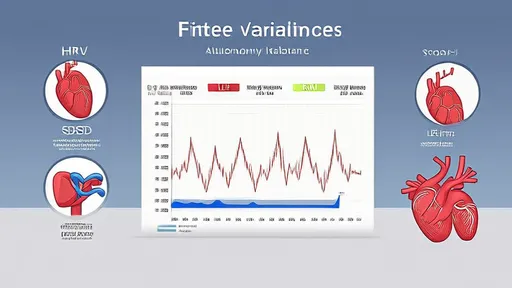
Sleep quality and duration profoundly influence metabolic health in ways we're only beginning to fully understand. Chronic sleep deprivation triggers hormonal changes that promote insulin resistance, including elevated cortisol and reduced leptin levels. Establishing consistent sleep patterns and achieving 7-9 hours of quality sleep nightly helps regulate the body's glucose metabolism and appetite hormones.
Dietary patterns play perhaps the most crucial role in determining insulin sensitivity. The standard Western diet, high in refined carbohydrates and processed foods, directly contributes to insulin resistance. Shifting toward whole, nutrient-dense foods with balanced macronutrients creates a metabolic environment where insulin can function optimally. Particular attention should be paid to the quality and quantity of carbohydrates consumed, with emphasis on fiber-rich, low-glycemic options.
Emerging research highlights the importance of meal timing and frequency in metabolic regulation. Time-restricted eating, where food consumption occurs within a specific window each day, appears to enhance insulin sensitivity by aligning with our natural circadian rhythms. This approach gives the pancreas regular periods of rest from insulin secretion, potentially reducing metabolic stress.
Chronic stress represents an often-overlooked contributor to insulin resistance. When the body remains in a prolonged stressed state, cortisol and other stress hormones promote glucose release into the bloodstream while simultaneously making cells less responsive to insulin. Incorporating stress-reduction techniques such as meditation, deep breathing exercises, or mindful movement can help break this cycle.
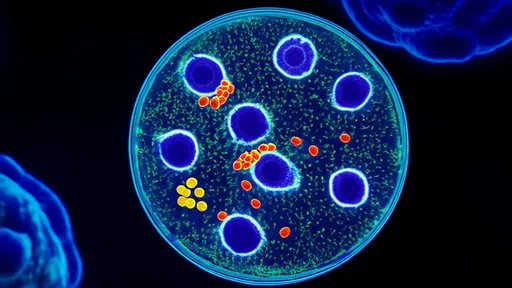
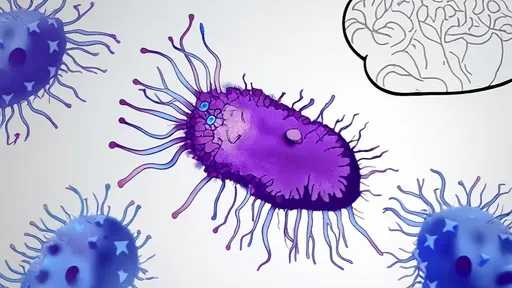
The gut microbiome has emerged as a surprising player in metabolic health. Certain gut bacteria influence how we metabolize food and regulate blood sugar. Fermented foods, prebiotic fibers, and a diverse plant-based diet support a healthy gut ecosystem that appears to enhance insulin sensitivity through various mechanisms, including reduced inflammation and improved gut barrier function.
Environmental toxins present in many everyday products may contribute to metabolic dysfunction. Chemicals like bisphenol A (BPA), phthalates, and certain pesticides have been linked to insulin resistance. Minimizing exposure by choosing fresh, organic foods when possible, using glass instead of plastic containers, and selecting natural personal care products may support metabolic health.
Hydration status influences blood viscosity and circulation, which in turn affects how efficiently glucose can reach cells. Even mild dehydration can temporarily increase blood sugar concentrations. Drinking adequate water throughout the day supports optimal metabolic function and may help maintain healthy insulin sensitivity.
Cold exposure through methods like cold showers or controlled cryotherapy may stimulate brown adipose tissue activity. This special fat tissue burns glucose for heat generation, potentially improving glucose metabolism and insulin sensitivity. While research is still developing in this area, the metabolic benefits of moderate cold exposure appear promising.
Social connections and community engagement might seem unrelated to insulin sensitivity, but loneliness and social isolation correlate with poorer metabolic health. Positive social interactions reduce stress and often encourage healthier lifestyle choices, creating an indirect but meaningful impact on insulin function.
Implementing these strategies requires a personalized approach, as individual responses vary based on genetics, current health status, and lifestyle factors. The cumulative effect of multiple small changes often proves more sustainable and effective than drastic overhauls. Monitoring progress through methods like continuous glucose monitoring or regular blood tests can provide valuable feedback for refinement.
The journey toward improved insulin sensitivity without medication isn't about perfection but rather consistent application of evidence-based practices. Each positive choice creates metabolic momentum, gradually restoring the body's natural ability to manage blood sugar effectively. This holistic approach not only enhances insulin sensitivity but typically improves overall health and vitality in the process.
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025