Chronic inflammation has emerged as a critical factor in the pathogenesis of numerous diseases, ranging from cardiovascular disorders to neurodegenerative conditions. The ability to detect and monitor inflammation through molecular markers has revolutionized both clinical diagnostics and therapeutic interventions. Unlike acute inflammation, which is a transient and protective response, chronic inflammation persists over time, often silently damaging tissues and organs. Identifying reliable biomarkers for chronic inflammation is essential for early diagnosis, prognosis, and personalized treatment strategies.
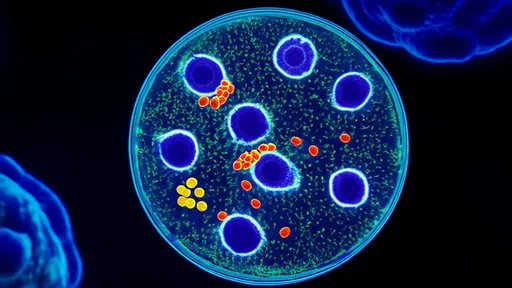
Recent advances in molecular biology and immunology have uncovered a wide array of biomarkers associated with chronic inflammation. Among the most well-studied are C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α). These markers are not only indicative of ongoing inflammatory processes but also correlate with disease severity and progression. For instance, elevated CRP levels have been linked to an increased risk of atherosclerosis, while IL-6 and TNF-α are often elevated in autoimmune diseases such as rheumatoid arthritis and inflammatory bowel disease.
The detection of these biomarkers relies on sophisticated laboratory techniques, including enzyme-linked immunosorbent assays (ELISAs), multiplex immunoassays, and more recently, high-throughput sequencing technologies. Each method offers unique advantages in terms of sensitivity, specificity, and scalability. However, challenges remain in standardizing these assays across different laboratories and populations. Variability in sample collection, storage, and processing can significantly impact the accuracy and reproducibility of biomarker measurements.
Beyond the conventional markers, researchers are exploring novel biomarkers that could provide deeper insights into the mechanisms of chronic inflammation. For example, microRNAs (miRNAs) and extracellular vesicles (EVs) have shown promise as non-invasive indicators of inflammatory status. These molecules can reflect tissue-specific changes and offer a more dynamic view of inflammation compared to traditional protein-based markers. Additionally, advances in metabolomics and proteomics are enabling the discovery of new biomarkers that were previously undetectable with older technologies.
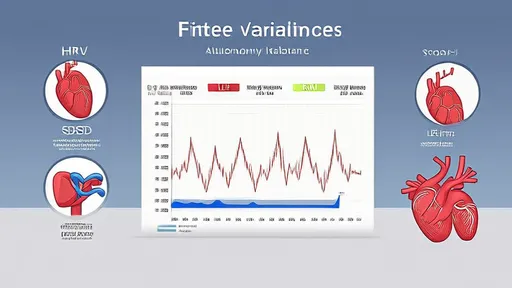
The clinical utility of inflammation biomarkers extends beyond diagnosis. They are increasingly being used to monitor treatment responses and predict patient outcomes. In oncology, for instance, inflammatory markers can indicate how a patient is responding to immunotherapy or chemotherapy. Similarly, in chronic inflammatory diseases like lupus or psoriasis, biomarker levels can guide dose adjustments and therapeutic switches. This personalized approach not only improves patient care but also reduces the risk of adverse effects from unnecessary or ineffective treatments.
Despite the progress, there are still gaps in our understanding of how these biomarkers interact with each other and with the underlying disease processes. Chronic inflammation is a complex and multifaceted phenomenon, often involving multiple pathways and feedback loops. Future research should focus on integrating data from different biomarkers to create comprehensive inflammatory profiles. Such profiles could help distinguish between different subtypes of chronic inflammation and identify patients who are most likely to benefit from targeted therapies.
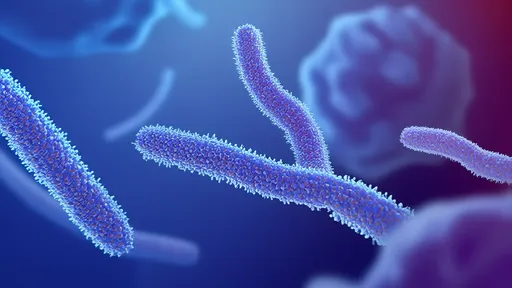
Another area of growing interest is the role of the microbiome in modulating chronic inflammation. Emerging evidence suggests that gut bacteria can influence systemic inflammation through the production of metabolites and other signaling molecules. This has led to the exploration of microbiome-derived biomarkers, which could offer a more holistic view of inflammation and its impact on health. Combining microbiome data with traditional inflammatory markers may open new avenues for diagnostics and therapeutics.
In conclusion, the field of chronic inflammation biomarkers is rapidly evolving, driven by technological advancements and a deeper understanding of inflammatory pathways. While challenges remain, the potential benefits of these markers in improving patient outcomes are undeniable. As research continues to uncover new biomarkers and refine existing ones, the hope is that we will move closer to a future where chronic inflammation can be detected, monitored, and treated with unprecedented precision.
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025